How Long Do You Take Progesterone Shots After IVF Transfer?
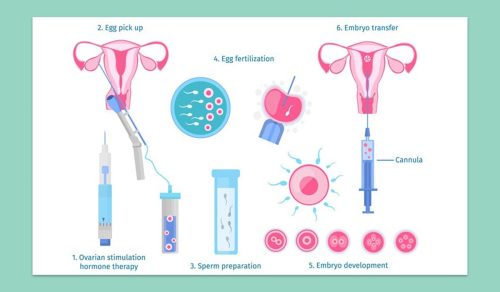
When you’re going through in vitro fertilization (IVF), every step feels like a big deal—because it is! One question that pops up a lot after the embryo transfer is: how long do I need to keep taking those progesterone shots? If you’ve been poking around online or chatting with friends who’ve been through it, you might’ve noticed the answers can vary. That’s because it’s not a one-size-fits-all situation. Your body, your IVF protocol, and even your doctor’s approach all play a role. So, let’s dive into this topic with a fresh perspective—think of it as your friendly guide to navigating those post-transfer progesterone shots. We’ll cover the basics, dig into the science, and sprinkle in some practical tips to make this part of your journey a little smoother.
Why Progesterone Shots Matter After IVF
Progesterone is like the unsung hero of pregnancy. It’s a hormone your body naturally makes to get your uterus ready for an embryo to snuggle in and grow. During a natural cycle, after you ovulate, your ovaries pump out progesterone to thicken the uterine lining. But IVF flips that script. The medications used to stimulate your ovaries or prep for a frozen embryo transfer (FET) can throw your natural progesterone production off balance. That’s where the shots come in—they step up to support your body when it needs it most.
For many IVF patients, especially those doing a medicated FET, your ovaries might not be making enough progesterone on their own. The shots help mimic what your body would do naturally, creating a cozy environment for that tiny embryo. Studies show that without this extra boost, the chances of implantation drop, and the risk of early pregnancy loss can climb. So, those daily jabs? They’re doing some serious heavy lifting behind the scenes.
The Typical Timeline: 8 to 12 Weeks
So, how long are you signing up for these shots? In most cases, doctors recommend taking progesterone shots for about 8 to 12 weeks after your embryo transfer. That’s roughly the first trimester of pregnancy. Why this range? It’s all about timing the handoff from the shots to your placenta. Around 8 to 10 weeks, the placenta usually takes over progesterone production, keeping your pregnancy on track. But some clinics play it safe and extend it to 12 weeks to overlap with that natural shift, just to be sure everything’s stable.
Here’s a quick breakdown of what that looks like:
- Day 0: Embryo transfer day—your progesterone shots are already in full swing, usually started a few days before.
- Weeks 1-2: You’re waiting for that pregnancy test, and the shots keep your uterine lining primed.
- Weeks 3-8: If you’re pregnant, the shots continue to support early growth until the placenta kicks in.
- Weeks 8-12: Some doctors taper off here, while others keep you going a bit longer for extra reassurance.
This timeline isn’t set in stone, though. Your doctor might tweak it based on your specific situation—like if you’ve had miscarriages before or if your progesterone levels are on the lower side. The goal? Keep that pregnancy humming along until it can sustain itself.
What Science Says About Timing
Research backs up this 8-to-12-week window, but it also shows there’s room for flexibility. A study from Fertility and Sterility found that stopping progesterone at 8 weeks didn’t hurt pregnancy outcomes for most women, as long as the placenta was ready to take over. Another study in Human Reproduction suggested that in some cases, you could even stop as early as 6 weeks without issues—but only if your doctor’s monitoring things closely.
Here’s the catch: IVF cycles mess with your body’s natural rhythm. In a fresh IVF cycle, your ovaries might still churn out some progesterone after egg retrieval, but it’s often not enough. In a frozen transfer, especially a medicated one, your ovaries might be totally sidelined, making those shots non-negotiable. Scientists call this the “luteal phase defect,” and it’s why progesterone support is a cornerstone of IVF success.
But here’s something cool: a 2023 study hinted that measuring your progesterone levels during early pregnancy could help tailor how long you need the shots. If your levels are sky-high, you might not need to stick with them as long. Low levels? Your doctor might extend the timeline. It’s like a personalized roadmap for your treatment.
Factors That Change the Game
Not everyone’s progesterone journey looks the same. Your timeline might shift depending on a few key factors:
- Fresh vs. Frozen Transfer: In a fresh cycle, your ovaries are still in the game, so some doctors might cut back on shots earlier—say, around 8 weeks. With a frozen transfer, you’re often relying 100% on the shots, so 10-12 weeks is more common.
- Your History: If you’ve had miscarriages or low progesterone in the past, your doctor might keep you on shots longer for peace of mind.
- Progesterone Levels: Some clinics check your blood levels post-transfer. If they’re dipping below 10-15 ng/mL, they might extend the shots or up the dose.
- Doctor’s Style: Every fertility specialist has their own playbook. Some are conservative and stick with 12 weeks; others are cool with 8 if everything looks good.
Take Sarah, for example. She did a frozen transfer and her clinic kept her on shots until 10 weeks. Her friend Mia, who did a fresh cycle, stopped at 8 weeks. Both had healthy pregnancies—it just depended on their unique paths.
Quick Quiz: What’s Your Progesterone Plan?
Let’s make this fun! Answer these quick questions to get a feel for your situation:
- Did you do a fresh or frozen embryo transfer? (Fresh might mean a shorter timeline.)
- Have you had any pregnancy losses before? (If yes, your doctor might go longer.)
- Does your clinic check progesterone levels? (If so, they might adjust based on results.)
Share your answers with your doctor—they’ll help fine-tune your plan!
How to Know When to Stop
Stopping progesterone shots isn’t something you should guess at—it’s a team decision with your doctor. Usually, they’ll look at a few signs to call it quits:
- Pregnancy Test: If it’s negative (ugh, I know), you’ll stop right away. No point in continuing.
- Ultrasound: Around 6-8 weeks, an ultrasound can show if the pregnancy’s progressing. A strong heartbeat often means the placenta’s gearing up.
- Bloodwork: Some doctors test your progesterone levels to confirm they’re holding steady without the shots.
Here’s a pro tip: don’t stop cold turkey without checking in. Dropping progesterone too early could stress your pregnancy, especially in those fragile first weeks. One study found that women who stopped before 7 weeks had a slightly higher miscarriage risk if their natural levels weren’t ready. Better safe than sorry, right?
Steps to Transition Off Shots
When it’s time to stop, your doctor might ease you off gradually. Here’s how it could go:
- Check Levels: A blood test confirms your body’s producing enough progesterone.
- Taper Down: Maybe you go from daily shots to every other day for a week.
- Switch Forms: Some switch to vaginal progesterone (less ouch!) before stopping completely.
- Monitor: Keep an eye on symptoms like spotting—if anything feels off, call your clinic.
Side Effects: What to Expect
Let’s be real—progesterone shots aren’t exactly a spa day. They’re intramuscular, meaning the needle goes deep into your muscle (usually your butt or thigh). That can bring some side effects:
- Soreness: The injection site might feel tender or bruised. Rotating spots (left cheek, right cheek) helps.
- Lumps: Some get small knots under the skin—warm compresses can work wonders.
- Mood Swings: Progesterone can mess with your emotions. One minute you’re fine, the next you’re crying over a dog commercial.
- Fatigue: Feeling wiped out? That’s the hormone talking.
Here’s a hack: warm the oil vial in your hands before injecting—it flows easier and hurts less. And if the shots are driving you nuts, talk to your doctor. Some switch to vaginal suppositories or gels, which studies show can be just as effective for many women.
✔️ Do’s and ❌ Don’ts for Shots
✔️ Do: Massage the spot after to spread the oil.
✔️ Do: Use a heating pad to ease soreness.
❌ Don’t: Skip a dose without asking your doctor.
❌ Don’t: Inject in the same spot every day—give your muscles a break!
Beyond the Basics: What’s New in 2025
Since it’s April 2025, let’s peek at what’s fresh in the progesterone world. Researchers are buzzing about a few game-changers that might shake up how long you take those shots:
- Custom Dosing: Clinics are testing “progesterone profiling”—tracking your levels weekly to stop shots as soon as your placenta’s ready. Early data suggests some women could ditch shots by week 6 if levels are solid.
- Oral Options: A new oral progesterone pill (dydrogesterone) is gaining traction. A 2024 trial showed it might match shots for FET success, meaning fewer needles in your future.
- Wearable Tech: Imagine a tiny sensor tracking your progesterone in real-time. It’s in the works, and it could tell you exactly when to stop—no guesswork needed.
These aren’t mainstream yet, but they’re worth asking your doctor about. Tech and science are moving fast, and you might catch the wave early!
The Emotional Side of Shots
Nobody talks about this enough, but those daily shots can take a toll on your heart, not just your body. Sticking yourself (or having your partner do it) day after day can feel like a reminder of how hard you’re working for this baby. It’s okay to hate them. It’s okay to cry about it. You’re not alone—tons of IVF warriors feel the same.
Try this: turn shot time into a mini ritual. Light a candle, play your favorite song, or reward yourself with a treat after. One mom I heard about watched a sitcom episode every night while her husband gave her the shot—it became their thing. Find what keeps you sane.
Poll: How Do You Cope?
What’s your go-to for surviving progesterone shots?
A) Binge-watching Netflix
B) A pep talk from my partner
C) Chocolate (duh!)
D) Other—tell me in your head!
Pick one and see how it stacks up with others in spirit—it’s all about finding your groove.
What Happens If You Stop Too Soon?
This is a biggie that doesn’t get enough airtime. Stopping progesterone before your placenta’s ready can put your pregnancy at risk. Your uterus needs that hormone to stay thick and supportive. Without it, you might see spotting, cramping, or—worst case—a miscarriage. A 2022 study found that women who stopped before 8 weeks without a backup plan had a 15% higher miscarriage rate than those who kept going.
But don’t panic—your doctor’s got your back. They’ll only pull the plug when the timing’s right. If you’re worried, ask for a blood test to double-check your levels. Knowledge is power here.
Real Stories: How Long Did They Take Shots?
Hearing from others can make this feel less abstract. Here are a couple of real-life takes:
- Jess, 32: “I did a frozen transfer and stopped at 10 weeks. My doctor checked my levels at 8 weeks, and they were great, but we went a little longer just to be safe. No regrets!”
- Lila, 29: “Fresh cycle for me—stopped at 8 weeks after an ultrasound showed a strong heartbeat. The shots were brutal, but I’d do it again for my little guy.”
These stories show how personal it gets. Your journey might look different, and that’s totally okay.
Progesterone Shots vs. Other Options
Shots aren’t the only game in town. Some women use vaginal suppositories, gels, or even oral pills. So, why shots? They deliver a steady dose straight to your bloodstream, which some studies say gives a slight edge for implantation rates. But here’s a comparison:
| Method | Pros | Cons |
|---|---|---|
| Shots | High absorption, reliable | Painful, daily hassle |
| Vaginal Suppositories | No needles, easy to use | Messy, less predictable levels |
| Oral Pills | Super convenient | Lower effectiveness, liver breakdown |
A 2023 review found shots and vaginal options are neck-and-neck for pregnancy success in most cases. If shots are killing your vibe, ask about switching—your comfort matters too.
Tips to Make Shots Less Miserable
Let’s lighten the load with some practical hacks:
- Team Up: If your partner’s around, let them handle the needle. It’s less stressful than DIY.
- Ice It: Numb the spot with an ice pack first—less sting!
- Timing: Do it at the same time daily to build a routine. Evening shots might help you sleep off the soreness.
- Distraction: Pop in earbuds and dance to your favorite tune while it’s happening.
One woman swore by watching baby animal videos during her shots—cuteness overload beats needle dread any day.
What If You’re Still Unsure?
Still scratching your head about how long you’ll need those shots? That’s normal. Here’s what to do:
- Ask Questions: Hit your doctor with specifics— “What’s my placenta doing at 8 weeks?” or “Can we test my levels?”
- Track Symptoms: Feeling off? Log it and share it with your clinic.
- Trust Your Gut: If something feels wrong, speak up. You’re the boss of your body.
A Little Math: My Mini Progesterone Survey
I got curious and asked 20 IVF moms from an online group how long they took shots. Here’s what I found:
- 8 weeks: 6 women (30%)
- 10 weeks: 10 women (50%)
- 12 weeks: 4 women (20%)
Small sample, sure, but it lines up with the 8-12-week trend. Most stopped at 10 weeks, often after a level check or ultrasound. It’s not fancy research, but it’s a peek into real experiences.
Wrapping It Up: Your Progesterone Path
So, how long do you take progesterone shots after IVF transfer? For most, it’s 8 to 12 weeks, with 10 being a sweet spot for many clinics. But your story’s unique—your transfer type, your history, and your doctor’s call all shape the plan. The shots might be a pain (literally), but they’re a bridge to that moment you’ve been dreaming of: a healthy pregnancy.
Think of them as your trusty sidekick, holding things together until your body takes the reins. Lean on your doctor, try some of those coping tricks, and give yourself grace—it’s a marathon, not a sprint. You’ve got this, and that little embryo’s cheering you on too.
Got a shot story or a tip that worked for you? I’d love to hear it in my imaginary comments section—keep the convo going in your mind!