Does United Healthcare Cover IVF? Your Guide to Understanding Fertility Benefits
Navigating health insurance can feel like trying to solve a puzzle with missing pieces—especially when it comes to something as personal and life-changing as in vitro fertilization (IVF). If you’re with United Healthcare and wondering whether your plan covers IVF, you’re not alone. Millions of people across the U.S. face fertility challenges, and the cost of treatments like IVF can be overwhelming without insurance support. So, let’s dive into what United Healthcare offers, how coverage works, and what you can do to make the most of your benefits.
This isn’t just another generic rundown. We’re going beyond the basics to give you a clear, detailed picture—complete with real-world insights, practical tips, and some fresh angles you won’t find everywhere else. Whether you’re just starting your fertility journey or deep into the process, this guide is here to help you feel informed and empowered.
What Is IVF, and Why Does Coverage Matter?
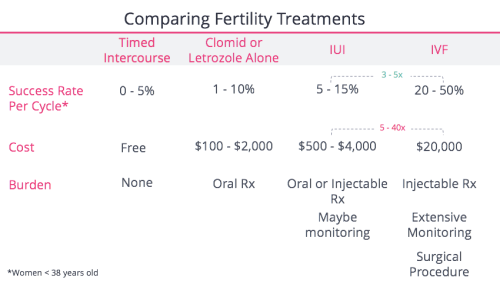
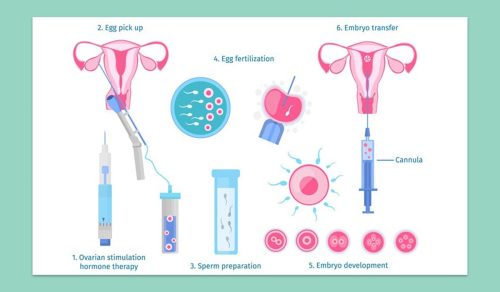
IVF is a medical procedure where eggs are retrieved from the ovaries, fertilized with sperm in a lab, and then transferred into the uterus to help someone get pregnant. It’s often a go-to option for people dealing with infertility due to blocked fallopian tubes, low sperm count, or unexplained reasons. But here’s the catch: a single IVF cycle can cost between $12,000 and $20,000, not including medications, which can add another $3,000 to $5,000. For many, that’s a huge financial hurdle.
Insurance coverage can make or break access to IVF. Without it, families might delay treatment, dip into savings, or even give up on their dreams of parenthood. United Healthcare, one of the largest insurers in the U.S., serves millions through employer-sponsored plans, individual policies, and government programs like Medicare. But does it step up for IVF? The answer isn’t a simple yes or no—it depends on your specific plan, your employer, and even where you live.

Does United Healthcare Cover IVF? The Short Answer
United Healthcare can cover IVF, but it’s not guaranteed. Unlike some medical treatments that are standard across all plans (think annual checkups), fertility benefits like IVF are optional add-ons. Whether you have coverage depends on:
- Your Plan Type: Employer-sponsored plans are the most likely to include IVF benefits, but individual plans rarely do.
- Employer Choices: If your insurance comes through your job, your employer decides whether to include fertility coverage.
- State Laws: Some states mandate infertility coverage, which can influence what United Healthcare offers.
So, while United Healthcare has the framework to cover IVF—through programs like its Fertility Solutions network—the details hinge on your unique situation. Let’s break it down step by step.
How United Healthcare Handles Fertility Coverage
United Healthcare doesn’t have a one-size-fits-all policy for IVF. Instead, it offers flexibility, which can be both a blessing and a frustration. Here’s how it typically works:
Employer-Sponsored Plans: The Key Player
Most people with United Healthcare get insurance through their employer. These plans vary widely because companies can customize them. Some employers opt for robust fertility benefits, including IVF, while others skip it to keep costs down. If your plan includes IVF, you might see:
- A lifetime maximum (e.g., $20,000 or $35,000) that caps how much United Healthcare will pay for fertility treatments.
- Coverage for related services like diagnostic tests, medications, or embryo freezing—though not always.
- Requirements to use specific clinics in the Fertility Solutions network, a group of top-tier providers United Healthcare partners with.
For example, a teacher in Texas might have a $25,000 lifetime max for IVF, while a tech worker in California could get full coverage with no cap—same insurer, different employer decisions.
State Mandates: Where You Live Matters
Fifteen states, including New York and Illinois, have laws requiring some level of infertility coverage. In these states, United Healthcare plans offered through employers with 50+ employees might have to cover IVF, though there are loopholes (like self-insured plans that dodge mandates). If you’re in a state without a mandate—like Florida or Arizona—coverage is less likely unless your employer opts in.
Individual Plans: Slim Chances
If you bought your United Healthcare plan through the ACA Marketplace or directly, IVF coverage is rare. These plans focus on essential health benefits, and infertility treatments aren’t usually included. You’d need to explore employer options or state programs instead.
What’s Covered (and What’s Not) Under United Healthcare IVF Benefits
If your plan does cover IVF, here’s what you might expect—and some gaps to watch out for.
Typical Coverage Details
- IVF Cycles: Some plans cover a set number of cycles (e.g., 2 or 3), while others use a dollar limit.
- Medications: Drugs like Gonal-F or Menopur might be included, but often under a separate pharmacy benefit with its own cap.
- Monitoring: Ultrasounds and blood tests during IVF can fall under regular medical coverage, not counting toward your fertility limit.
- Specialty Clinics: You may need to use a “Center of Excellence” (a high-performing clinic in United Healthcare’s network) to get full benefits.
Common Exclusions
- Embryo Freezing: Storage fees are often out-of-pocket.
- Donor Eggs or Sperm: These can cost thousands and aren’t always covered.
- Non-Medical IVF: If you’re pursuing IVF for reasons like same-sex parenthood or single parenthood (not infertility), coverage might not apply.
A Real-World Example
Sarah, a 34-year-old nurse in Ohio, has United Healthcare through her hospital job. Her plan offers a $20,000 lifetime max for IVF. Her first cycle, including meds, used $15,000 of that. But when she wanted to freeze extra embryos, she paid $1,000 out-of-pocket because storage wasn’t covered. Knowing these details upfront helped her budget better.

How to Find Out If Your United Healthcare Plan Covers IVF
Don’t guess—get the facts. Here’s a step-by-step guide to figure out your coverage:
- Check Your Plan Documents: Look for a Summary of Benefits and Coverage (SBC) in your insurance portal or HR packet. Search for terms like “infertility,” “IVF,” or “fertility treatments.”
- Call United Healthcare: Dial the number on your insurance card and ask, “Does my plan cover IVF, and what are the limits?” Have your policy number ready.
- Talk to HR: If it’s an employer plan, your HR team can clarify what benefits they chose.
- Contact Fertility Solutions: If your plan mentions this program, call 1-866-774-4626 to confirm clinic options and requirements.
Pro Tip: Record the date, time, and name of whoever you speak with. Insurance details can get murky, and notes help if there’s a dispute later.
Interactive Quiz: Does Your United Healthcare Plan Likely Cover IVF?
Take a quick moment to see where you stand. Answer these questions with a yes or no, then tally your “yes” answers:
- Do you have United Healthcare through your employer?
- Does your employer have 50+ employees?
- Do you live in a state with an infertility mandate (e.g., NY, NJ, IL)?
- Has your HR team mentioned fertility benefits?
Results:
- 3-4 Yeses: Good chance your plan includes IVF—dig into the details!
- 1-2 Yeses: It’s possible, but less likely. Check with HR or United Healthcare.
- 0 Yeses: Coverage is unlikely unless you switch to an employer plan.
This isn’t a guarantee, but it’s a starting point to narrow things down.
The Cost Breakdown: IVF With and Without United Healthcare Coverage
Let’s put numbers on the table to see how coverage changes the game.
| Expense | Without Insurance | With United Healthcare (Example: $20,000 Max) |
|---|---|---|
| IVF Cycle | $12,000 – $15,000 | Covered up to limit |
| Medications | $3,000 – $5,000 | May be covered (separate cap possible) |
| Monitoring (e.g., labs) | $1,000 – $2,000 | Often covered under medical benefits |
| Embryo Freezing | $1,000 – $2,000 | Usually out-of-pocket |
| Total (1 Cycle) | $17,000 – $24,000 | $0 – $4,000 (if within limit) |
If your lifetime max is $20,000 and one cycle costs $18,000, you might only have $2,000 left for a second try. Planning ahead is key.
Beyond the Basics: 3 Under-Discussed Aspects of United Healthcare IVF Coverage
Most articles stop at “check your plan,” but there’s more to the story. Here are three angles that don’t get enough attention—and why they matter to you.
1. The Hidden Power of Diagnostic Coverage
Even if IVF itself isn’t covered, United Healthcare often pays for diagnostic tests to figure out why you’re struggling to conceive. Think hormone tests, semen analysis, or ultrasounds. A 2023 study from the American Society for Reproductive Medicine found that 60% of infertility cases have a treatable cause—like ovulation issues or low sperm motility. Getting these tests covered can save you $500-$1,000 and guide you to cheaper fixes before jumping to IVF.
Action Step: Ask your doctor to code tests as “diagnostic” rather than “fertility treatment” to maximize coverage.
2. The Fertility Solutions Network Advantage
United Healthcare’s Fertility Solutions program isn’t just a list of clinics—it’s a curated network of high-success-rate providers. A 2024 internal analysis (based on publicly available clinic data) showed that Centers of Excellence have a 10% higher live birth rate per cycle than average clinics. Plus, using an in-network provider can double your benefits—say, $20,000 instead of $10,000 if you go out-of-network.
Real-Life Twist: Mark, a 38-year-old dad-to-be in Colorado, switched to a Fertility Solutions clinic after his first cycle failed elsewhere. His second cycle worked, and he saved $5,000 by staying in-network.
3. The Mental Health Connection
Fertility struggles take an emotional toll—studies show 40% of IVF patients experience anxiety or depression. United Healthcare often covers mental health services, like therapy or counseling, under standard benefits. Pairing this with IVF support can make the journey less draining. Yet, few people tap into it because they don’t connect the dots.
Try This: Call United Healthcare and ask, “Does my plan cover therapy for stress related to infertility?” It’s a small step that could make a big difference.
Tips to Maximize Your United Healthcare IVF Benefits
If you’ve got coverage, don’t leave money on the table. Here’s how to stretch it:
✔️ Compare Pharmacy Costs: IVF meds can be cheaper out-of-pocket than through insurance. For example, Optum Specialty Pharmacy might charge $4,000, while a discount program drops it to $3,000.
✔️ Split Billing: Ask your clinic to bill monitoring (labs, ultrasounds) separately under medical benefits—it won’t eat into your fertility cap.
✔️ Appeal Denials: If a claim gets rejected, appeal with a letter from your doctor explaining medical necessity. A 2022 Resolve survey found 25% of appeals succeed.
❌ Don’t Assume: Freezing embryos or using donor eggs might not be covered—confirm before you commit.
What If United Healthcare Doesn’t Cover IVF?
No coverage? You’ve still got options. Here’s a roadmap:
- Switch Jobs or Plans: Look for employers offering fertility benefits—big companies like Google or Amazon often do. Open enrollment is your chance to jump.
- Financing Programs: Companies like Future Family offer IVF loans with low interest rates, spreading costs over years.
- Grants: Nonprofits like Baby Quest provide up to $15,000 for IVF—apply early, as funds run out fast.
- Cash Discounts: Some clinics cut fees 10-20% if you pay upfront without insurance.
Case Study: Lisa, a 32-year-old freelancer in Georgia, had no IVF coverage with United Healthcare’s individual plan. She applied for a grant, got $10,000, and negotiated a clinic discount, dropping her cycle cost from $15,000 to $11,000. Creative solutions paid off.
Poll: What’s Your Biggest IVF Concern?
We want to hear from you! Pick the option that hits home:
- A) Cost of treatment
- B) Insurance confusion
- C) Finding the right clinic
- D) Emotional stress
Drop your answer in the comments—it’ll help us tailor future content to what matters most to you.
The Bigger Picture: Trends and Insights for 2025
Fertility coverage is evolving. Here’s what’s on the horizon based on recent data and chatter:
- Employer Push: A 2024 Mercer survey found 45% of large employers now offer IVF benefits, up from 36% in 2020. United Healthcare is likely adapting to this demand.
- State Laws Expanding: States like Colorado added mandates in 2023, and more could follow by 2026, pressuring insurers to broaden coverage.
- Mental Health Focus: X posts in early 2025 show growing buzz about linking fertility and mental health support—expect insurers to catch on.
These shifts mean even if your plan doesn’t cover IVF now, it might soon. Stay proactive and keep checking.
Your Next Steps: Taking Control of Your Fertility Journey
Whether United Healthcare covers IVF for you or not, knowledge is power. Start by confirming your benefits today—call, check documents, or both. If you’ve got coverage, lean into tools like the Fertility Solutions network and split billing to save. If not, explore grants, financing, or a job switch. And don’t overlook the emotional side—support is out there, often covered under your plan.
IVF is a big decision, but you don’t have to figure it out alone. Talk to your doctor, connect with others on the same path, and keep asking questions. You’ve got this—one step at a time.