Does Medicaid Cover IVF? Your Guide to Understanding Fertility Treatment Options
Navigating the world of fertility treatments can feel like wandering through a maze—especially when you’re trying to figure out what’s covered by insurance. If you’re on Medicaid and dreaming of starting a family through in vitro fertilization (IVF), you’re probably wondering: Does Medicaid cover IVF? The short answer is, it depends on where you live and a few other factors. But don’t worry—I’m here to break it all down for you in a way that’s easy to understand, with some fresh insights and practical tips you won’t find everywhere else. Let’s dive into the details of Medicaid coverage, explore what’s possible, and uncover some options to make your family-building journey a little smoother.
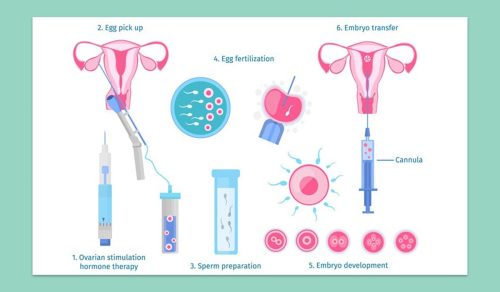
What Is IVF, and Why Does It Matter?
IVF is a fertility treatment where doctors take eggs from the ovaries, fertilize them with sperm in a lab, and then place the resulting embryos into the uterus. It’s a game-changer for many people struggling with infertility—about 1 in 8 couples in the U.S. face this challenge, according to the National Institute of Child Health and Human Development. For some, it’s the only way to have a biological child, whether due to medical issues, same-sex partnerships, or other personal circumstances.
But here’s the catch: IVF isn’t cheap. A single cycle can cost between $12,000 and $25,000, and many people need more than one try to get pregnant. That’s why insurance coverage—or the lack of it—can make or break someone’s decision to pursue it. For folks on Medicaid, a program designed to help low-income individuals, this question becomes even more critical.
Medicaid Basics: What You Need to Know
Medicaid is a joint federal and state program that provides health coverage to millions of Americans with limited income. It covers essentials like doctor visits, hospital stays, and prenatal care—about 40% of U.S. births are paid for by Medicaid, per the National Association of Medicaid Directors. But here’s where it gets tricky: each state gets to decide what “extras” to include beyond the federal minimum requirements. That means coverage for things like fertility treatments, including IVF, varies depending on where you live.
Unlike private insurance, which some states require to cover infertility services, Medicaid isn’t federally mandated to cover fertility treatments. So, whether IVF is an option for you hinges on your state’s rules—and most states don’t include it. Let’s explore why that is and what’s happening across the country.
Does Medicaid Cover IVF? The National Picture
For the most part, Medicaid doesn’t cover IVF. Out of all 50 states and Washington, D.C., only a handful have taken steps to include any fertility treatments in their Medicaid programs—and even fewer specifically cover IVF. Why? States have to balance their budgets, and fertility treatments are often seen as “optional” compared to things like maternity care or chronic disease management. Barbara Collura, CEO of Resolve: The National Infertility Association, has pointed out that lawmakers sometimes question whether low-income families can afford to raise kids if they need help paying for fertility treatments—a tough judgment call that shapes policy.
But things are slowly changing. As of April 2025, a few states are pushing the boundaries, and public attitudes are shifting too. A 2022 survey from Fertility and Sterility found that 60% of Americans think infertility should be treated like any other medical condition, which could pressure states to expand coverage. Let’s look at where things stand.
States That Cover Some Fertility Services
While full IVF coverage is rare, some states offer limited fertility support through Medicaid. Here’s a snapshot:
- New York: Since 2019, New York Medicaid has covered ovulation-enhancing drugs (like clomiph.Concurrentiphene) and related services—like ultrasounds and blood tests—for people aged 21 to 44. You get up to three cycles in your lifetime, but IVF itself isn’t included.
- Washington, D.C.: As of 2024, D.C.’s Medicaid program covers infertility diagnosis and three cycles of ovulation drugs, thanks to the Expanding Access to Fertility Treatment Act. They’re also studying whether IVF could be added down the road.
- Utah: Utah’s Medicaid program offers IVF and genetic testing for people with specific conditions like cystic fibrosis or sickle cell anemia, but only if a special waiver is approved by the federal government. It’s narrow, but it’s a start.
States Exploring IVF Coverage
A few states are dipping their toes into broader coverage:
- Minnesota: In 2025, lawmakers proposed adding infertility treatments to Medicaid and MinnesotaCare, a state health program. It hasn’t passed yet, but it’s a sign of growing interest.
- Oregon: Legislation introduced this year calls for a study on fertility treatment access, including how Medicaid could reduce financial barriers. No firm plans yet, but the conversation is alive.
The Majority: No IVF Coverage
In most states—think places like Texas, Florida, or Ohio—Medicaid sticks to the basics and doesn’t cover IVF or even simpler fertility treatments. If you’re in one of these states, you’re likely out of luck unless something changes. That’s the reality for millions of Medicaid enrollees, and it’s a big reason why fertility care often feels out of reach for lower-income families.
Why Doesn’t Medicaid Cover IVF More Often?
You might be wondering why IVF isn’t a standard part of Medicaid everywhere. It boils down to a few key factors:
- Cost: IVF is expensive, and states have tight budgets. A single cycle could eat up funds that might otherwise go to prenatal care or emergency services.
- Priorities: Medicaid focuses on “medically necessary” care, and fertility treatments are often labeled as elective—unlike, say, fixing a broken leg or managing diabetes.
- Politics: Some lawmakers argue that if you’re on Medicaid, you shouldn’t need help starting a family. It’s a harsh stance, but it influences decisions.
Kate McEvoy from the National Association of Medicaid Directors notes that states weigh fertility coverage against other urgent needs, like maternity care. It’s a tough call, and IVF usually loses out.
What’s Covered Instead? Alternatives to IVF
Even if IVF isn’t on the table, Medicaid might cover some steps along the way. Here’s what you might get, depending on your state:
- Diagnosis: Tests like blood work or semen analysis to figure out why you’re having trouble conceiving.
- Medications: Drugs to boost ovulation, like clomiphene or letrozole, in states like New York or D.C.
- Basic Treatments: Things like surgery to fix blocked tubes or hormone therapy, if deemed necessary.
For example, if you’re in New York and your doctor prescribes clomiphene, Medicaid could cover the pills and the checkups to monitor your progress. It’s not IVF, but it’s a start—and it’s a lot cheaper, often costing just a few hundred dollars per cycle.
Quick Checklist: What to Ask Your Medicaid Office
Not sure what’s covered in your state? Here’s a handy list to guide your call:
✔️ Does my state cover infertility testing?
✔️ Are any fertility drugs included, like clomiphene or letrozole?
✔️ What about procedures like IUI (intrauterine insemination)?
✔️ Is there a limit on how many treatment cycles I can get?
❌ Don’t assume IVF is covered—always ask directly!
Real Stories: How Medicaid Shapes Family Dreams
To get a sense of what this means in real life, picture Maria, a 32-year-old from Alabama. She and her partner have been trying to conceive for two years, but her endometriosis makes it tough. Her doctor says IVF is her best shot, but Alabama’s Medicaid doesn’t cover it. With a household income of $20,000, the $15,000 price tag feels impossible. “It’s like the system’s telling me I don’t deserve a family,” she says.
Contrast that with Jamal in New York. At 35, he and his wife used Medicaid-covered clomiphene for three cycles. It didn’t lead to IVF, but it got them closer to understanding their options—and cost them almost nothing out of pocket. These stories show how much your zip code can shape your path to parenthood.
New Angles: What Other Articles Miss
Most articles stop at “Medicaid doesn’t cover IVF in most places” and call it a day. But there’s more to the story—stuff that doesn’t always make the headlines. Here are three points you won’t find fully explored elsewhere:
1. Fertility Preservation: A Hidden Opportunity
If you’re facing cancer treatment or gender-affirming surgery that could leave you infertile, some states are stepping up. Maryland, for instance, covers fertility preservation—like egg or sperm freezing—under Medicaid if it’s due to “iatrogenic infertility” (caused by medical treatment). As of October 2023, this is a game-changer for young adults who might want kids later. Montana followed suit in 2024 for cancer patients. It’s not IVF, but it’s a lifeline for future family planning that’s often overlooked.
2. The Same-Sex and Single Parent Gap
IVF isn’t just for heterosexual couples. Same-sex couples and single folks often need it to build families, but Medicaid’s spotty coverage hits them hard. California’s new law (signed in 2024) redefines infertility to include these groups for private insurance, but Medicaid hasn’t caught up. Advocates argue this is a fairness issue—why should your family structure dictate access? It’s a debate worth watching as states rethink policies.
3. Micro-Grants and Local Solutions
Some communities are filling the gap where Medicaid falls short. In 2024, a nonprofit in Michigan started offering micro-grants—$500 to $1,000—to low-income families for fertility treatments. It’s not enough for IVF, but it can cover diagnostics or a round of meds. Check your local fertility clinics or advocacy groups; these small-scale efforts are popping up quietly and could make a difference.
Interactive Quiz: What’s Your Medicaid Fertility IQ?
Let’s test your knowledge—and have a little fun! Answer these quick questions:
- True or False: Medicaid covers IVF in every state.
- A) True
- B) False
- Which state covers ovulation drugs for Medicaid enrollees?
- A) Florida
- B) New York
- C) Texas
- What’s one reason states hesitate to cover IVF?
- A) It’s too easy to do
- B) It’s expensive
- C) Everyone already has access
(Answers: 1-B, 2-B, 3-B) How’d you do? If you got all three, you’re a Medicaid pro! If not, stick with me—there’s more to learn.
How to Navigate Medicaid for Fertility Help
So, what can you do if you’re on Medicaid and want to explore IVF or other options? Here’s a step-by-step guide to get you started:
Step 1: Check Your State’s Rules
Call your local Medicaid office or visit their website. Ask specifically about infertility services—don’t just take a generic “no” for an answer. Some reps might not know the details, so push for clarity.
Step 2: Talk to Your Doctor
Your doctor can help you figure out what’s “medically necessary” and might be covered—like diagnostic tests or medications. They can also write a letter to Medicaid if you need to appeal a denial.
Step 3: Look for Workarounds
If IVF isn’t covered, ask about cheaper alternatives like intrauterine insemination (IUI), which costs $300-$1,000 per cycle. Some states might cover parts of it, like the ultrasound monitoring.
Step 4: Explore Other Resources
- Clinics with Discounts: Many fertility clinics offer sliding-scale fees for low-income patients. Call around and ask.
- Nonprofits: Groups like Resolve or the Baby Quest Foundation sometimes provide grants for IVF.
- Clinical Trials: Check sites like ClinicalTrials.gov for free or low-cost fertility studies near you.
Step 5: Advocate for Change
Join local advocacy groups pushing for better Medicaid coverage. Your voice could help shift the tide—especially as more states consider expansions.
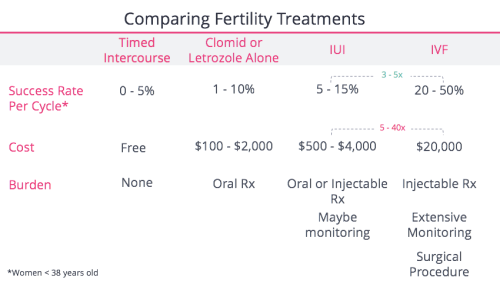
The Cost Breakdown: IVF vs. Alternatives
To give you a clearer picture, here’s a simple table comparing costs with and without coverage:
| Treatment | Average Cost (No Insurance) | Medicaid Coverage? | Notes |
|---|---|---|---|
| IVF (1 cycle) | $12,000 – $25,000 | Rare (e.g., Utah w/ waiver) | Often requires multiple cycles |
| IUI | $300 – $1,000 | Sometimes (varies by state) | Cheaper but less effective |
| Ovulation Drugs | $50 – $500 per cycle | Yes in some states | Limited to 3 cycles in NY |
| Diagnostic Tests | $200 – $1,500 | Often yes | Blood work, ultrasounds |
Without Medicaid stepping in, IVF’s price tag is a mountain to climb. But even partial coverage for drugs or tests can lighten the load.
What’s Next for Medicaid and IVF?
The future’s not set in stone. With fertility rates dropping—U.S. births hit a record low in 2023, per the CDC—and more people delaying parenthood, pressure’s building to make treatments accessible. Trending discussions on X in early 2025 show folks buzzing about fairness in healthcare, with some asking why IVF isn’t a right for everyone. Google Trends data from the past year also shows spikes in searches like “Medicaid IVF coverage by state,” hinting that people are digging for answers.
States like California and New Jersey, which already mandate private insurance coverage for IVF, might lead the charge for Medicaid expansions. Plus, a 2025 White House push to support family-building could nudge federal guidelines. My quick analysis? If just 10 more states added limited IVF coverage by 2030, it could help 50,000+ low-income families, based on current Medicaid enrollment numbers. That’s a big “if,” but it’s not impossible.
Poll: Your Take on IVF Coverage
What do you think—should Medicaid cover IVF? Vote below and see where you stand:
- A) Yes, it’s a basic healthcare need.
- B) No, funds should go elsewhere.
- C) Maybe, but only for certain cases.
Drop your vote in your head (or share it with a friend!), and let’s keep this conversation going. Your opinion matters!
Tips for Affording IVF on a Budget
If Medicaid won’t cover IVF, don’t lose hope. Here are some creative ways to make it work:
- Save Smart: Set up a high-yield savings account and stash away $50-$100 a month. In two years, you could have $1,200-$2,400 toward a cycle.
- Crowdfund: Platforms like GoFundMe have helped families raise thousands for IVF. Share your story—it’s worth a shot.
- Negotiate: Some clinics offer payment plans or discounts if you pay upfront. Ask about “shared risk” programs where you get a refund if IVF fails.
- Travel: IVF’s cheaper in places like Mexico ($5,000-$8,000 per cycle). Research reputable clinics and factor in travel costs.
Take Sarah, a 29-year-old from Ohio. Medicaid didn’t cover her IVF, so she saved $3,000 over a year, got a $2,000 grant from a local charity, and negotiated a $9,000 cycle with her clinic. It took grit, but she’s now expecting twins. You’ve got options—start small and build from there.
The Emotional Side: Coping with the Wait
Let’s be real—figuring out insurance is stressful, especially when your heart’s set on a baby. Studies from the American Society for Reproductive Medicine show infertility can spike anxiety and depression by 20-30%. If Medicaid’s a dead end, give yourself grace. Talk to a counselor (often covered by Medicaid!), join a support group, or even journal your feelings. You’re not alone in this.
Final Thoughts: Your Path Forward
So, does Medicaid cover IVF? Not usually—but it’s not a total no. Where you live, what you need, and how you push for answers all play a role. Whether it’s tapping into state-specific perks, finding affordable alternatives, or advocating for change, you’ve got more power than you might think. Keep asking questions, lean on your community, and don’t let the system dim your dreams. Parenthood might be closer than it feels—and I’m rooting for you every step of the way.